Datuk Dr Suresh, ID Physician of Hospital Sungai Buloh has given a very insightful webinar organized by the Malaysia Medical Association on 16/2/22 concerning the Omicron wave. Here are some take home messages which are useful and practical for us:
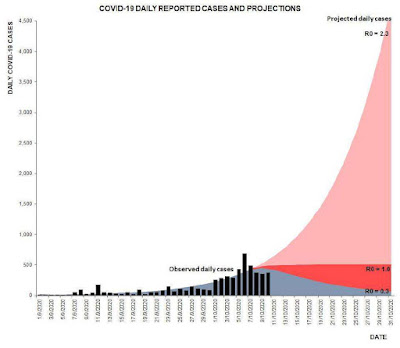
- A sharp spike of Omicron cases is expected. However after we have reached the peak, there will be a sharp drop in cases as well.
- Be prepared for episodic spikes every now and then. We will have to manage with Omicron amongst us (towards endemicity).
- Omicron has taken over Delta. Although Omicron spreads faster, it causes less hospitalization and ICU admissions compared to Delta variant.
- Omicron spreads much faster than the Wuhan or Delta variant because of the shorter incubation period (about 3 days). It also takes approximately 2-3 days for a person who started to have covid symptoms to cause another person to start having covid symptoms as well.
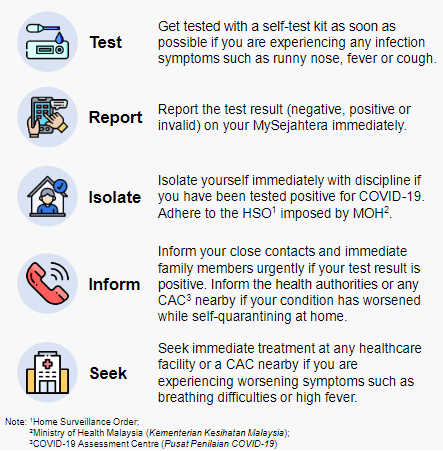
- There is no perfect covid test. A highly sensitive test like PCR can cause unnecessary quarantine for people with low viral load who are not infectious. A less sensitive test like RTK-Ag (swab or salive self-test kit) might miss some positive cases with high viral load (yet below the detection threshold), thus escaping quarantine. Therefore close contact history and symptoms evolution must be considered also in making sense of the test results.
- Although Omicron has proven to be less aggressive than Delta variant, the highest risk group for severe outcome are:
- ≥ 40 years old with comorbid, unvaccinated
- ≥ 60 years old with comorbid irrespective of vaccine status
This algorithm applies to HCW who had covid infection before and now fully recovered. A healthcare worker who does not have symptoms within 90 days after recovery from covid infection can continue to work without restrictions and does not require testing after low risk close contact. This is because the HCW's neutralizing antibodies are presumably high post covid infection within the first 90 days.
LOW RISK close contact is if both you and the source person are WEARING MASKS. A source person is someone who is confirmed positive for COVID-19.IF YOU DO NOT HAVE SYMPTOMS:
- You do not require RTK-Ag testing to return to work.
- However, you are required to self-monitor for the next 14 days.
- At any point within the 14 days period if symptoms develop, do an RTK-Ag test.
- Do RTK-Ag test immediately.
- You can return to work if your RTK-Ag is NEGATIVE.
- If required, continue re-evaluating symptoms to decide if medical leave is required until symptoms resolve or go for further testing ie PCR to have a conclusive diagnosis.
- A 14-day duration for self-monitoring of symptoms is required.
- You need to do RTK-Ag as soon as you are aware of such exposure.
- If your test result is NEGATIVE, then you can return to work.
- DAILY RTK-Ag TESTING is required until Day 5 post exposure for those fully vaccinated or until Day 7 post exposure for those partially/unvaccinated. You can work as long as you are tested negative.
- Continue self-monitoring for symptoms until Day 14.
- You should not go to work yet. Do RTK-Ag test immediately AND at Day 3 post exposure.
- If at Day 3 RTK-Ag test is NEGATIVE and SYMPTOMS RESOLVE, then only you can return to work.
- If symptoms persist till Day 3 but RTK-Ag is negative, then do a PCR before returning to work.
- DAILY RTK-Ag TESTING is required until Day 5 post exposure for those fully vaccinated or until Day 7 post exposure for those partially/unvaccinated. You can work as long as you are tested negative.
- Continue self-monitoring for symptoms until Day 14.